Health
FDA approves HIV ‘prevention’ pill
AIDS activists divided over benefit versus risk of Truvada
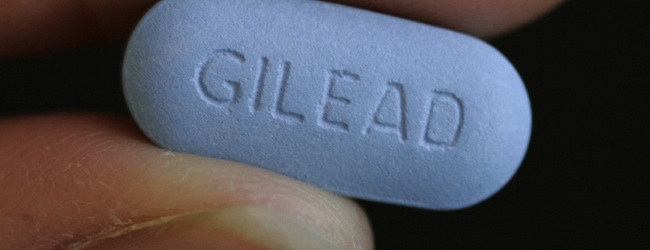
The U.S. Food and Drug Administration on Monday announced it has approved use of the AIDS drug Truvada for reducing the risk of HIV infection among uninfected people considered at high risk for contracting HIV through sexual contact.
The decision to allow Truvada to be taken daily in the form of a pill as part of a prevention regimen known as pre-exposure prophylaxis, or “PrEP,” has drawn mixed reactions among AIDS advocacy organizations, with most supporting the decision.
But others have raised strong objections, saying potentially harmful side effects of Truvada along with the risk of HIV infection through non-adherence to a rigid daily drug regimen, which in turn could lead to drug-resistant strains of HIV, far outweigh the benefits.
“Today’s approval marks an important milestone in our fight against HIV,” said FDA Commissioner Dr. Margaret Hamburg. “Every year, about 50,000 U.S. adults and adolescents are diagnosed with HIV infection, despite the availability of prevention methods and strategies to educate, test, and care for people living with the disease,” she said.
“New treatments as well as prevention methods are needed to fight the HIV epidemic in this country,” Hamburg said.
Truvada, which is manufactured by the pharmaceutical firm Gilead Sciences, was first approved in 2004 by the FDA for use as a treatment for HIV.
In announcing its approval for use as a prevention drug, the FDA pointed to two large placebo-controlled trials of the drug as a prophylaxis that were sponsored by the U.S. National Institutes of Health and the University of Washington.
One of the trials conducted in the U.S. and abroad evaluated the drug in 2,400 HIV-negative men or transgender women who have sex with men and who are prone to “high risk behavior,” such as inconsistent or no condom use during sex, according to a statement released by the FDA.
“Results showed Truvada was effective in reducing the risk of HIV infection by 42 percent compared with [a] placebo in this population,” the FDA statement says.
It says the second trial included 4,759 heterosexual couples where one partner was HIV-infected and the other was HIV negative. Truvada reduced the risk of becoming infected by 75 percent compared to participants taking a placebo, the FDA statement says.
Among those supporting the FDA decision to approve Truvada as a prevention drug is Project Inform, the San Francisco based HIV patient advocacy group that has closely observed prevention and treatment options for people with HIV and AIDS for more than 20 years.
“Project Inform is extremely pleased with a landmark decision by the FDA to approve the first biomedical HIV prevention product in the history of the epidemic,” the group said in a statement.
“Finally, after 30 years, HIV-negative individuals have a new way to protect themselves from becoming infected,” said Project Inform Director Dana Van Gorder. “While PrEP isn’t a tool that will be appropriate for broad use, we are thrilled to have a new option that could offer substantial benefit to those at highest risk for HIV, including gay and bisexual men and transgender women who struggle with consistent condom use, and in heterosexual women living in areas with high HIV rates whose partners refuse to use condoms,” Van Gorder said.
The AIDS Institute, a national AIDS advocacy group with offices in Washington, D.C. and Florida, and the Boston-based Fenway Health and its research arm Fenway Institute also issued statements supporting the FDA action.
Taking the opposite view is the Los Angeles based AIDS Healthcare Foundation, which provides HIV/AIDS treatment programs in the U.S. and in countries throughout the world, including Africa and Asia.
“My initial reaction is that this is a catastrophe for AIDS prevention in the U.S.,” said Michael Weinstein, AHF’s executive director.
Weinstein said global trial studies cited by the FDA involved constant monitoring and encouragement by organizers to ensure that participants adhered to their daily drug regimen as well as engaged in safer sex practices, such as condom use.
“The bottom line is that was under ideal conditions,” he said. “People were tested monthly. They were intensively counseled. They were paid to be in the study. And only about 50 percent took the drug.”
He predicted far fewer people “in the real world” would be compliant in taking their daily drug regimen, especially since the drug, as reported by Gilead Sciences, induces occasional side effects in healthy people such as headache, stomach discomfort and weight loss.
Weinstein said that in addition to opening the way for users to lower their guard and stop using condoms, even though the FDA approval calls for continued use of safer sex practices along with Truvada, the drug is highly dangerous for people who become HIV positive without knowing it.
In its published drug warnings, Gilead says use of Truvada alone is harmful to people with HIV unless they use it in combination with other antiretroviral drugs. Weinstein said he fears that people using Truvada as a prevention pill and become HIV positive after failing to take the drug every day could be at high risk – both for becoming ill and developing a drug resistant strain of HIV.
Dr. Debra Brinkrant, an FDA official who has monitored the Truvada studies, said an analysis of the trial studies showed that those who used Truvada used condoms more frequently and did not discontinue condom use.
“Everyone has to work together to make sure this works,” she said. “We must see that adherence is maintained. This is a first step to cut the infection rate,” a rate she said has not decreased in spite of years of other HIV prevention and education programs.
Justin Goforth, director of medical adherence and head of the Sexually Transmitted Disease Clinic at D.C.’s Whitman-Walker Health, said Whitman-Walker has already been prescribing Truvada as a prevention pill as part of a small study program. He said Whitman-Walker will likely expand the number of people it approves for use of the drug as a prevention medication now that the FDA has issued its approval.
“A lot of gay men are coming in and begging us to get this,” he said. “This is clearly not for everyone. The issue is finding the right people. They have to be people at high risk,” he said, adding that men who have sex with men who themselves or their partners have trouble being complaint with condom use, or those with multiple sex partners, would be among those considered for Truvada as a prevention pill.
Goforth acknowledged that the NIH sponsored trials of Truvada for men who have sex with men and transgender women had an adherence rate of about 50 percent. The fact that they were paid to be in the trials could have been responsible for the low adherence rate, with many choosing to join the program for the purpose of taking the money rather than the pills, Goforth said.
But he said Whitman-Walker has found through its limited Truvada trial program for HIV negative people that those seeking out the drug have followed the daily pill regimen.
“I feel people who come forward now to take this have a greater incentive for compliance,” he said.
And Goforth pointed to studies showing that Truvada’s effectiveness in preventing HIV infection is greater than 90 percent among those who take the pill every day.
Monkeypox
US contributes more than $90 million to fight mpox outbreak in Africa
WHO and Africa CDC has declared a public health emergency
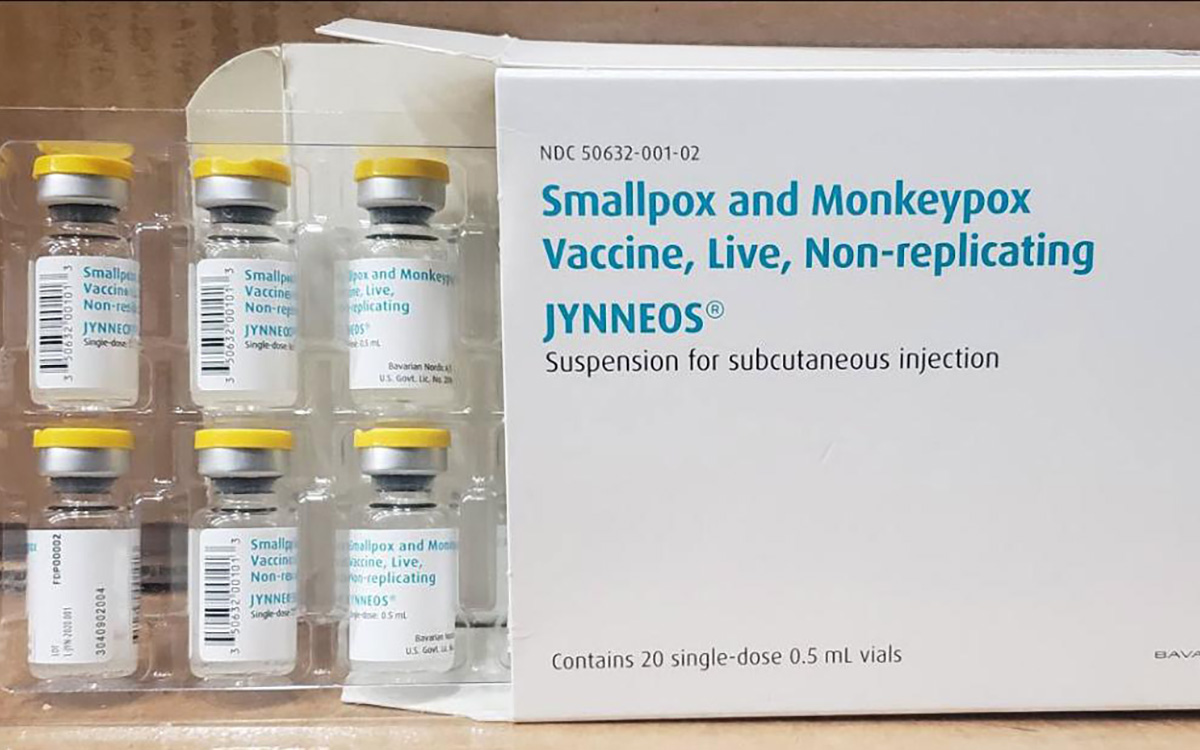
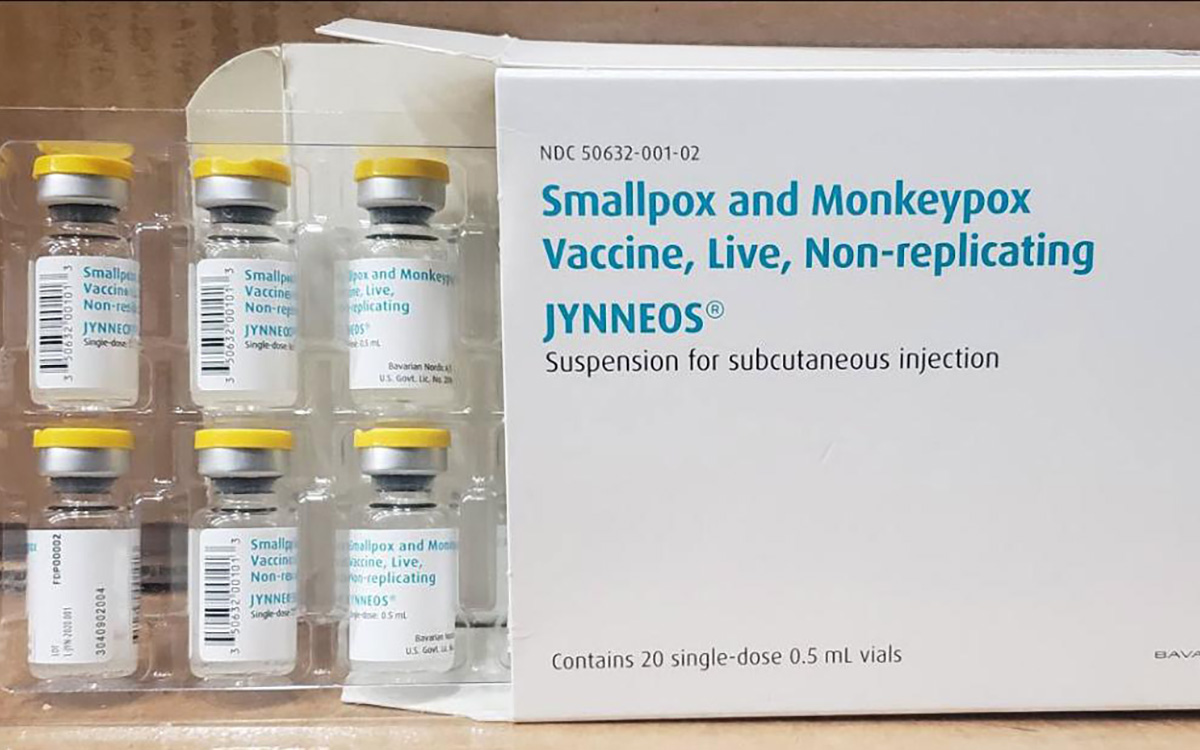
The U.S. has contributed more than $90 million to the fight against the mpox outbreak in Africa.
The U.S. Agency for International Development on Tuesday in a press release announced “up to an additional” $35 million “in emergency health assistance to bolster response efforts for the clade I mpox outbreak in Central and Eastern Africa, pending congressional notification.” The press release notes the Biden-Harris administration previously pledged more than $55 million to fight the outbreak in Congo and other African countries.
“The additional assistance announced today will enable USAID to continue working closely with affected countries, as well as regional and global health partners, to expand support and reduce the impact of this outbreak as it continues to evolve,” it reads. “USAID support includes assistance with surveillance, diagnostics, risk communication and community engagement, infection prevention and control, case management, and vaccination planning and coordination.”
The World Health Organization and the Africa Centers for Disease Control and Prevention last week declared the outbreak a public health emergency.
The Washington Blade last week reported there are more than 17,000 suspected mpox cases across in Congo, Uganda, Kenya, Rwanda, and other African countries. The outbreak has claimed more than 500 lives, mostly in Congo.
Health
Mpox outbreak in Africa declared global health emergency
ONE: 10 million vaccine doses needed on the continent
Medical facilities that provide treatment to gay and bisexual men in some East African countries are already collaborating with them to prevent the spread of a new wave of mpox cases after the World Health Organization on Wednesday declared a global health emergency.
The collaboration, both in Uganda and Kenya, comes amid WHO’s latest report released on Aug. 12, which reveals that nine out of every 10 reported mpox cases are men with sex as the most common cause of infection.
The global mpox outbreak report — based on data that national authorities collected between January 2022 and June of this year — notes 87,189 of the 90,410 reported cases were men. Ninety-six percent of whom were infected through sex.
Sexual contact as the leading mode of transmission accounted for 19,102 of 22,802 cases, followed by non-sexual person-to-person contact. Genital rash was the most common symptom, followed by fever and systemic rash.
The WHO report states the pattern of mpox virus transmission has persisted over the last six months, with 97 percent of new cases reporting sexual contact through oral, vaginal, or anal sex with infected people.
“Sexual transmission has been recorded in the Democratic Republic of Congo among sex workers and men who have sex with men,” the report reads. “Among cases exposed through sexual contact in the Democratic Republic of the Congo, some individuals present only with genital lesions, rather than the more typical extensive rash associated with the virus.”
The growing mpox cases, which are now more than 2,800 reported cases in at least 13 African countries that include Kenya, Uganda, Rwanda, and prompted the Africa Centers for Disease Control and Prevention this week to declare the disease a public health emergency for resource mobilization on the continent to tackle it.
“Africa has long been on the frontlines in the fight against infectious diseases, often with limited resources,” said Africa CDC Director General Jean Kaseya. “The battle against Mpox demands a global response. We need your support, expertise, and solidarity. The world cannot afford to turn a blind eye to this crisis.”
The disease has so far claimed more than 500 lives, mostly in Congo, even as the Africa CDC notes suspected mpox cases across the continent have surged past 17,000, compared to 7,146 cases in 2022 and 14,957 cases last year.
“This is just the tip of the iceberg when we consider the many weaknesses in surveillance, laboratory testing, and contact tracing,” Kaseya said.
WHO, led by Director General Tedros Adhanom Ghebreyesus, also followed the Africa CDC’s move by declaring the mpox outbreak a public health emergency of international concern.
The latest WHO report reveals that men, including those who identify as gay and bisexual, constitute most mpox cases in Kenya and Uganda. The two countries have recorded their first cases, and has put queer rights organizations and health care centers that treat the LGBTQ community on high alert.
The Uganda Minority Shelters Consortium, for example, confirmed to the Washington Blade that the collaboration with health service providers to prevent the spread of mpox among gay and bisexual men is “nascent and uneven.”
“While some community-led health service providers such as Ark Wellness Clinic, Children of the Sun Clinic, Ice Breakers Uganda Clinic, and Happy Family Youth Clinic, have demonstrated commendable efforts, widespread collaboration on mpox prevention remains a significant gap,” UMSC Coordinator John Grace stated. “This is particularly evident when compared to the response to the previous Red Eyes outbreak within the LGBT community.”
Grace noted that as of Wednesday, there were no known queer-friendly health service providers to offer mpox vaccinations to men who have sex with men. He called for health care centers to provide inclusive services and a more coordinated approach.
Although Grace pointed out the fear of discrimination — and particularly Uganda’s Anti-Homosexuality Act — remains a big barrier to mpox prevention through testing, vaccination, and treatment among queer people, he confirmed no mpox cases have been reported among the LGBTQ community.
Uganda so far has reported two mpox cases — refugees who had travelled from Congo.
“We are for the most part encouraging safer sex practices even after potential future vaccinations are conducted as it can also be spread through bodily fluids like saliva and sweat,” Grace said.
Grace also noted that raising awareness about mpox among the queer community and seeking treatment when infected remains a challenge due to the historical and ongoing homophobic stigma and that more comprehensive and reliable advocacy is needed. He said Grindr and other digital platforms have been crucial in raising awareness.
The declarations of mpox as a global health emergency have already attracted demand for global leaders to support African countries to swiftly obtain the necessary vaccines and diagnostics.
“History shows we must act quickly and decisively when a public health emergency strikes. The current Mpox outbreak in Africa is one such emergency,” said ONE Global Health Senior Policy Director Jenny Ottenhoff.
ONE is a global, nonpartisan organization that advocates for the investments needed to create economic opportunities and healthier lives in Africa.
Ottenhoff warned failure to support the African countries with medical supplies needed to tackle mpox would leave the continent defenseless against the virus.
To ensure that African countries are adequately supported, ONE wants governments and pharmaceutical companies to urgently increase the provision of mpox vaccines so that the most affected African countries have affordable access to them. It also notes 10 million vaccine doses are currently needed to control the mpox outbreak in Africa, yet the continent has only 200,000 doses.
The Blade has reached out to Ishtar MSM, a community-based healthcare center in Nairobi, Kenya, that offers to service to gay and bisexual men, about their response to the mpox outbreak.
Health
White House urged to expand PrEP coverage for injectable form
HIV/AIDS service organizations made call on Wednesday
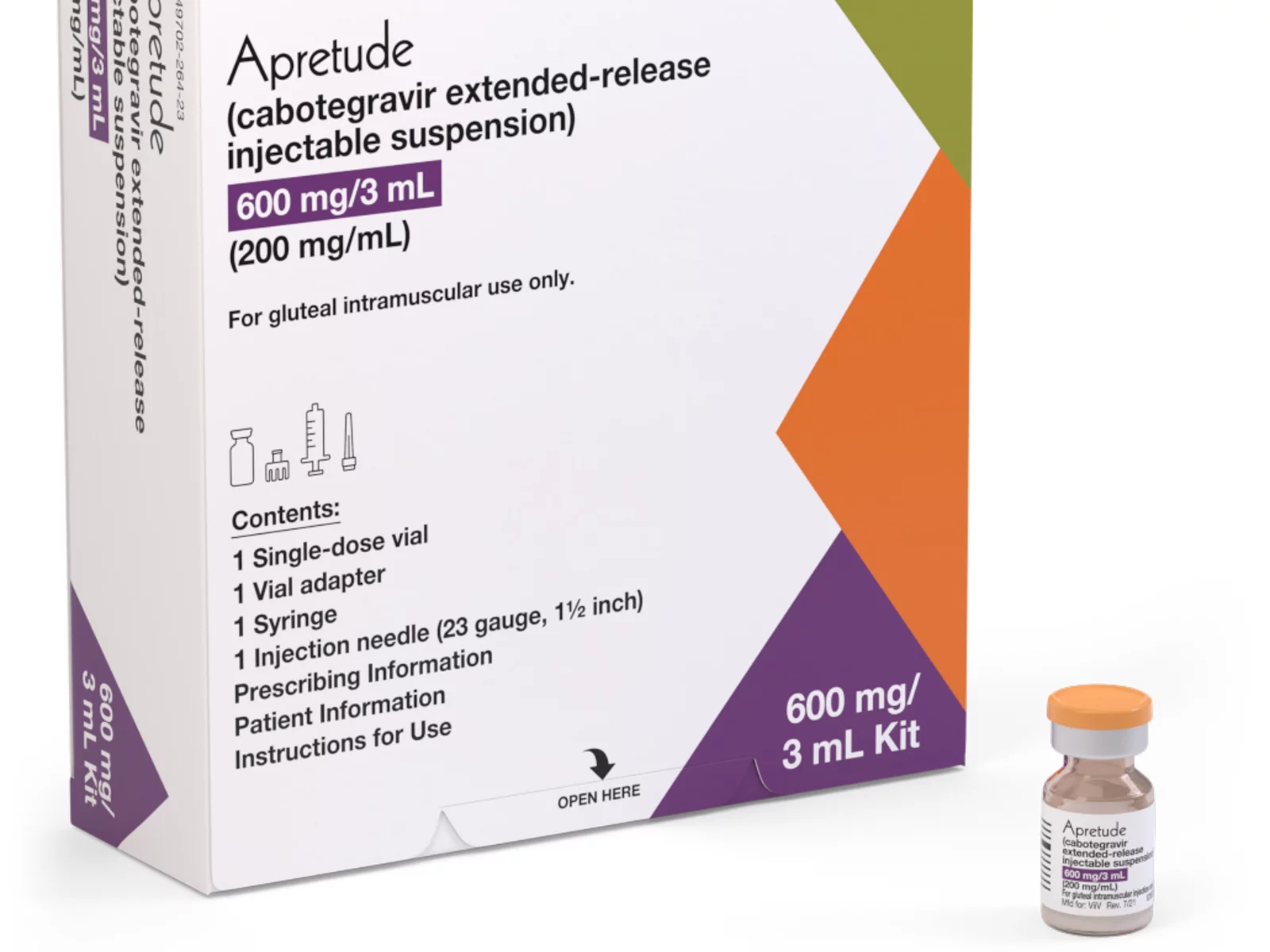
A coalition of 63 organizations dedicated to ending HIV called on the Biden-Harris administration on Wednesday to require insurers to cover long-acting pre-exposure prophylaxis (PrEP) without cost-sharing.
In a letter to Chiquita Brooks-LaSure, administrator of the Centers for Medicare and Medicaid Services, the groups emphasized the need for broad and equitable access to PrEP free of insurance barriers.
Long-acting PrEP is an injectable form of PrEP that’s effective over a long period of time. The FDA approved Apretude (cabotegravir extended-release injectable suspension) as the first and only long-acting injectable PrEP in late 2021. It’s intended for adults and adolescents weighing at least 77 lbs. who are at risk for HIV through sex.
The U.S. Preventive Services Task Force updated its recommendation for PrEP on Aug. 22, 2023, to include new medications such as the first long-acting PrEP drug. The coalition wants CMS to issue guidance requiring insurers to cover all forms of PrEP, including current and future FDA-approved drugs.
“Long-acting PrEP can be the answer to low PrEP uptake, particularly in communities not using PrEP today,” said Carl Schmid, executive director of the HIV+Hepatitis Policy Institute. “The Biden administration has an opportunity to ensure that people with private insurance can access PrEP now and into the future, free of any cost-sharing, with properly worded guidance to insurers.”
Currently, only 36 percent of those who could benefit from PrEP are using it. Significant disparities exist among racial and ethnic groups. Black people constitute 39 percent of new HIV diagnoses but only 14 percent of PrEP users, while Latinos represent 31 percent of new diagnoses but only 18 percent of PrEP users. In contrast, white people represent 24 percent of HIV diagnoses but 64 percent of PrEP users.
The groups also want CMS to prohibit insurers from employing prior authorization for PrEP, citing it as a significant barrier to access. Several states, including New York and California, already prohibit prior authorization for PrEP.
Modeling conducted for HIV+Hep, based on clinical trials of a once every 2-month injection, suggests that 87 percent more HIV cases would be averted compared to daily oral PrEP, with $4.25 billion in averted healthcare costs over 10 years.
Despite guidance issued to insurers in July 2021, PrEP users continue to report being charged cost-sharing for both the drug and ancillary services. A recent review of claims data found that 36 percent of PrEP users were charged for their drugs, and even 31 percent of those using generic PrEP faced cost-sharing.
The coalition’s letter follows a more detailed communication sent by HIV+Hepatitis Policy Institute to the Biden administration on July 2.
Signatories to the community letter include Advocates for Youth, AIDS United, Equality California, Fenway Health, Human Rights Campaign, and the National Coalition of STD Directors, among others.
-

 Opinions5 days ago
Opinions5 days agoIt’s time for new leadership on the Maryland LGBTQIA+ Commission
-

 The White House5 days ago
The White House5 days agoWhite House does not ‘respond’ to reporters’ requests with pronouns included
-

 Arts & Entertainment5 days ago
Arts & Entertainment5 days ago‘Gay is Good’ Pride Pils Can Celebrates Frank Kameny’s 100th Birthday for WorldPride in D.C.
-

 Sponsored5 days ago
Sponsored5 days agoTHC Drinks: What You Should Know About Cannabis Beverages