Health
AMA strengthens gender affirming care policies
Organization’s openly gay president sworn in on Tuesday

The American Medical Association on Monday voted to strengthen its policies governing access to gender affirming care for transgender and gender diverse individuals.
The group committed to opposing the criminalization of patients for seeking gender affirming care, and of families and healthcare providers for facilitating access to or administering that care.
Additionally, the AMA pledged to work with federal and state legislators and regulators to oppose policies criminalizing these guideline-directed healthcare interventions and to educate the Federation of State Medical Boards on their importance.
The resolution was introduced by the Endocrine Society, which issued a press release Monday celebrating the move: “As political attacks on gender-affirming care escalate, it is the responsibility of the medical community to speak out in support of evidence-based care.”
“Medical decisions should be made by patients, their relatives and health care providers, not politicians,” the Endocrine Society wrote.
The resolution was cosponsored by the American Academy of Pediatrics, the American College of Obstetricians and Gynecologists, the American Urological Association, the American Society for Reproductive Medicine, the American College of Physicians, the American Association of Clinical Endocrinology, GLMA: Health Professionals Advancing LGBTQ+ Equality and the AMA’s Medical Student Section.
The Endocrine Society explained the legislative bans on gender affirming care — passed in states in which 30 percent of the nation’s trans and gender-diverse youth now live — are misguided.
“Pediatric gender-affirming care is designed to take a conservative approach,” the group wrote.
“When young children experience feelings that their gender identity does not match the sex recorded at birth, the first course of action is to support the child in exploring their gender identity and to provide mental health support, as needed.”
“Medical intervention is reserved for older adolescents and adults, with treatment plans tailored to the individual and designed to maximize the time teenagers and their families have to make decisions about their transitions.
“Major medical organizations also agree on waiting until an individual has turned 18 or reached the age of majority in their country to undergo gender-affirming genital surgery.”
Additionally, the Endocrine Society noted research that shows gender affirming care can be lifesaving.
“A 2020 study analyzed survey data from 89 transgender adults who had access to puberty-delaying medication while adolescents and data from more than 3,400 transgender adults who did not. The study found that those who received puberty-delaying hormone treatment had lower likelihood of lifetime suicidal ideation than those who wanted puberty-delaying treatment but did not receive it, even after adjusting for demographic variables and level of family support.”
“Approximately nine in 10 transgender adults who wanted puberty-delaying treatment, but did not receive it, reported lifetime suicidal ideation.”
AMA inaugurates first gay president
Jesse Ehrenfeld, the AMA’s first openly gay president, was inaugurated during the 2023 Annual Meeting of House of Delegates on Tuesday.
An anesthesiologist who formerly served as the Joseph A. Johnson Jr. Distinguished Leadership Professor of anesthesiology, surgery, biomedical informatics and health policy at Vanderbilt University’s School of Medicine; Ehrenfeld spoke to the Washington Blade for an exclusive interview last month.
During his inaugural speech on Tuesday, Ehrenfeld relayed a personal story about how his now 4-year-old son, born early and severely underweight, needed a blood transfusion. “At this moment,” he said, “watching my son cling to life, I was struck by the painful reality that, even though I was a physician and now, a father … neither I, nor my husband, could donate blood — simply because we are gay.”
“Just recently, the FDA, thanks in large part to a decade of advocacy by our AMA and others, rescinded some of these discriminatory practices, making it possible for my husband and I to give someone else’s child a much-needed blood transfusion,” Ehrenfeld said. “This kind of advocacy is why I am so proud to lead our AMA at this moment.”
“Today there is an unconscionable effort to interfere in medicine,” Ehrenfeld said. “An assault on patient and physician autonomy. Legislative over-reach. Attacks on maternal health … on LGBTQ patients.”
“We have a duty to push back against legislative interference in the practice of medicine that is leading to the criminalization of care.”
Health
Young gay Latinos see rising share of new HIV cases, leading to call for targeted funding
Fernando Hermida diagnosed four months after asking for asylum

Four months after seeking asylum in the U.S., Fernando Hermida began coughing and feeling tired. He thought it was a cold. Then sores appeared in his groin and he would soak his bed with sweat. He took a test.
On New Year’s Day 2022, at age 31, Hermida learned he had HIV.
“I thought I was going to die,” he said, recalling how a chill washed over him as he reviewed his results. He struggled to navigate a new, convoluted health care system. Through an HIV organization he found online, he received a list of medical providers to call in D.C., where he was at the time, but they didn’t return his calls for weeks. Hermida, who speaks only Spanish, didn’t know where to turn.
By the time of Hermida’s diagnosis, the U.S. Department of Health and Human Services was about three years into a federal initiative to end the nation’s HIV epidemic by pumping hundreds of millions of dollars annually into certain states, counties, and U.S. territories with the highest infection rates. The goal was to reach the estimated 1.2 million people living with HIV, including some who don’t know they have the disease.
Overall, estimated new HIV infection rates declined 23 percent from 2012 to 2022. But a KFF Health News-Associated Press analysis found the rate has not fallen for Latinos as much as it has for other racial and ethnic groups.
While African Americans continue to have the highest HIV rates in the U.S. overall, Latinos made up the largest share of new HIV diagnoses and infections among gay and bisexual men in 2022, per the most recent data available, compared with other racial and ethnic groups. Latinos, who make up about 19 percent of the U.S. population, accounted for about 33 percent of new HIV infections, according to the Centers for Disease Control and Prevention.
The analysis found Latinos are experiencing a disproportionate number of new infections and diagnoses across the U.S., with diagnosis rates highest in the Southeast. Public health officials in Mecklenburg County, North Carolina, and Shelby County, Tennessee, where data shows diagnosis rates have gone up among Latinos, told KFF Health News and the AP that they either don’t have specific plans to address HIV in this population or that plans are still in the works. Even in well-resourced places like San Francisco, HIV diagnosis rates grew among Latinos in the last few years while falling among other racial and ethnic groups despite the county’s goals to reduce infections among Latinos.
“HIV disparities are not inevitable,” Robyn Neblett Fanfair, director of the CDC’s Division of HIV Prevention, said in a statement. She noted the systemic, cultural, and economic inequities — such as racism, language differences, and medical mistrust.
And though the CDC provides some funds for minority groups, Latino health policy advocates want HHS to declare a public health emergency in hopes of directing more money to Latino communities, saying current efforts aren’t enough.
“Our invisibility is no longer tolerable,” said Vincent Guilamo-Ramos, co-chair of the Presidential Advisory Council on HIV/AIDS
Lost without an interpreter
Hermida suspects he contracted the virus while he was in an open relationship with a male partner before he came to the U.S. In late January 2022, months after his symptoms started, he went to a clinic in New York City that a friend had helped him find to finally get treatment for HIV.
Too sick to care for himself alone, Hermida eventually moved to Charlotte to be closer to family and in hopes of receiving more consistent health care. He enrolled in an Amity Medical Group clinic that receives funding from the Ryan White HIV/AIDS Program, a federal safety-net plan that serves over half of those in the nation diagnosed with HIV, regardless of their citizenship status.
His HIV became undetectable after he was connected with case managers. But over time, communication with the clinic grew less frequent, he said, and he didn’t get regular interpretation help during visits with his English-speaking doctor. An Amity Medical Group representative confirmed Hermida was a client but didn’t answer questions about his experience at the clinic.
Hermida said he had a hard time filling out paperwork to stay enrolled in the Ryan White program, and when his eligibility expired in September 2023, he couldn’t get his medication.
He left the clinic and enrolled in a health plan through the Affordable Care Act marketplace. But Hermida didn’t realize the insurer required him to pay for a share of his HIV treatment.
In January, the Lyft driver received a $1,275 bill for his antiretroviral — the equivalent of 120 rides, he said. He paid the bill with a coupon he found online. In April, he got a second bill he couldn’t afford.
For two weeks, he stopped taking the medication that keeps the virus undetectable and intransmissible.
“Estoy que colapso,” he said. I’m falling apart. “Tengo que vivir para pagar la medicación.” I have to live to pay for my medication.
One way to prevent HIV is preexposure prophylaxis, or PrEP, which is regularly taken to reduce the risk of getting HIV through sex or intravenous drug use. It was approved by the federal government in 2012 but the uptake has not been even across racial and ethnic groups: CDC data show much lower rates of PrEP coverage among Latinos than among white Americans.
Epidemiologists say high PrEP use and consistent access to treatment are necessary to build community-level resistance.
Carlos Saldana, an infectious disease specialist and former medical adviser for Georgia’s health department, helped identify five clusters of rapid HIV transmission involving about 40 gay Latinos and men who have sex with men from February 2021 to June 2022. Many people in the cluster told researchers they had not taken PrEP and struggled to understand the health care system.
They experienced other barriers, too, Saldana said, including lack of transportation and fear of deportation if they sought treatment.
Latino health policy advocates want the federal government to redistribute funding for HIV prevention, including testing and access to PrEP. Of the nearly $30 billion in federal money that went toward things like HIV health care services, treatment, and prevention in 2022, only 4% went to prevention, according to a KFF analysis.
They suggest more money could help reach Latino communities through efforts like faith-based outreach at churches, testing at clubs on Latin nights, and training bilingual HIV testers.
Latino Rates Going Up
Congress has appropriated $2.3 billion over five years to the Ending the HIV Epidemic initiative, and jurisdictions that get the money are to invest 25 percent of it in community-based organizations. But the initiative lacks requirements to target any particular groups, including Latinos, leaving it up to the cities, counties, and states to come up with specific strategies.
In 34 of the 57 areas getting the money, cases are going the wrong way: Diagnosis rates among Latinos increased from 2019 to 2022 while declining for other racial and ethnic groups, the KFF Health News-AP analysis found.
Starting Aug. 1, state and local health departments will have to provide annual spending reports on funding in places that account for 30 percent or more of HIV diagnoses, the CDC said. Previously, it had been required for only a small number of states.
In some states and counties, initiative funding has not been enough to cover the needs of Latinos.
South Carolina, which saw rates nearly double for Latinos from 2012-2022, hasn’t expanded HIV mobile testing in rural areas, where the need is high among Latinos, said Tony Price, HIV program manager in the state health department. South Carolina can pay for only four community health workers focused on HIV outreach — and not all of them are bilingual.
In Shelby County, Tennessee, home to Memphis, the Latino HIV diagnosis rate rose 86 percent from 2012 to 2022. The health department said it got $2 million in initiative funding in 2023 and while the county plan acknowledges that Latinos are a target group, department director Michelle Taylor said: “There are no specific campaigns just among Latino people.”
Up to now, Mecklenburg County, North Carolina, didn’t include specific targets to address HIV in the Latino population — where rates of new diagnoses more than doubled in a decade but fell slightly among other racial and ethnic groups. The health department has used funding for bilingual marketing campaigns and awareness about PrEP.
Moving for medicine
When it was time to pack up and move to Hermida’s third city in two years, his fiancé, who is taking PrEP, suggested seeking care in Orlando, Fla.
The couple, who were friends in high school in Venezuela, had some family and friends in Florida, and they had heard about Pineapple Healthcare, a nonprofit primary care clinic dedicated to supporting Latinos living with HIV.
The clinic is housed in a medical office south of downtown Orlando. Inside, the mostly Latino staff is dressed in pineapple-print turquoise shirts, and Spanish, not English, is most commonly heard in appointment rooms and hallways.
“At the core of it, if the organization is not led by and for people of color, then we’re just an afterthought,” said Andres Acosta Ardila, the community outreach director at Pineapple Healthcare, who was diagnosed with HIV in 2013.
“¿Te mudaste reciente, ya por fin?” asked nurse practitioner Eliza Otero. Did you finally move? She started treating Hermida while he still lived in Charlotte. “Hace un mes que no nos vemos.” It’s been a month since we last saw each other.
They still need to work on lowering his cholesterol and blood pressure, she told him. Though his viral load remains high, Otero said it should improve with regular, consistent care.
Pineapple Healthcare, which doesn’t receive initiative money, offers full-scope primary care to mostly Latino males. Hermida gets his HIV medication at no cost there because the clinic is part of a federal drug discount program.
The clinic is in many ways an oasis. The new diagnosis rate for Latinos in Orange County, Florida, which includes Orlando, rose by about a third from 2012 through 2022, while dropping by a third for others. Florida has the third-largest Latino population in the U.S., and had the seventh-highest rate of new HIV diagnoses among Latinos in the nation in 2022.
Hermida, whose asylum case is pending, never imagined getting medication would be so difficult, he said during the 500-mile drive from North Carolina to Florida. After hotel rooms, jobs lost, and family goodbyes, he is hopeful his search for consistent HIV treatment — which has come to define his life the past two years — can finally come to an end.
“Soy un nómada a la fuerza, pero bueno, como me comenta mi prometido y mis familiares, yo tengo que estar donde me den buenos servicios médicos,” he said. I’m forced to be a nomad, but like my family and my fiancé say, I have to be where I can get good medical services.
That’s the priority, he said. “Esa es la prioridad ahora.”
KFF Health News and The Associated Press analyzed data from the U.S. Centers for Disease Control and Prevention on the number of new HIV diagnoses and infections among Americans ages 13 and older at the local, state, and national levels. This story primarily uses incidence rate data — estimates of new infections — at the national level and diagnosis rate data at the state and county level.
Bose reported from Orlando, Fla.. Reese reported from Sacramento, Calif. AP video journalist Laura Bargfeld contributed to this report.
The Associated Press Health and Science Department receives support from the Robert Wood Johnson Foundation. The AP is responsible for all content.
This article was produced by KFF Health News, which publishes California Healthline, an editorially independent service of the California Health Care Foundation.
A Project of KFF Health News and the Associated Press co-published by Univision Noticias
CREDITS:
Reporters: Vanessa G. Sánchez, Devna Bose, Phillip Reese
Cinematography: Laura Bargfeld
Photography: Laura Bargfeld, Phelan M. Ebenhack
Video Editing: Federica Narancio, Kathy Young, Esther Poveda
Additional Video: Federica Narancio, Esther Poveda
Web Production: Eric Harkleroad, Lydia Zuraw
Special thanks to Lindsey Dawson
Editors: Judy Lin, Erica Hunzinger
Data Editor: Holly Hacker
Social Media: Patricia Vélez, Federica Narancio, Esther Poveda, Carolina Astuya, Natalia Bravo, Juan Pablo Vargas, Kyle Viterbo, Sophia Eppolito, Hannah Norman, Chaseedaw Giles, Tarena Lofton
Translation: Paula Andalo
Copy Editing: Gabe Brison-Trezise
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF — an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Commentary
Asian American and LGBTQ: A Heritage of Pride
May is Asian American, Native Hawaiian and Pacific Islander Heritage Month
Asian Americans and Pacific Islanders (APIs) are the nation’s fastest growing racial minority group by 2040, one in 10 Americans will be of Asian ancestry. And, while many Americans think that anti-Asian hate and racism towards Asian Americans has disappeared, the community disagrees.
The Asian American Foundation which found that Asian Americans are continually subjected to hate, violence, and discrimination, baldly reveals that disparity.
- 33 percent of Americans think hate towards Asian Americans has increased in the past year, compared to 61 percent of Asian Americans themselves.
- In the past year, 32 percent of Asian Americans across the country reported being called a racial slur; 29 percent said they were verbally harassed or verbally abused.
- Southeast Asian Americans report even higher incidences of being subject to racial slurs (40 percent), verbal harassment or abuse (38 percent), and threats of physical assault (22 percent).
- Many Asian Americans live in a state of fear and anxiety with 41 percent of Asian American/ Native Hawaiian/Pacific Islander (AANHPI) believing they will likely be the victims of a physical attack due to their race, ethnicity, or religion. These numbers are disturbing.
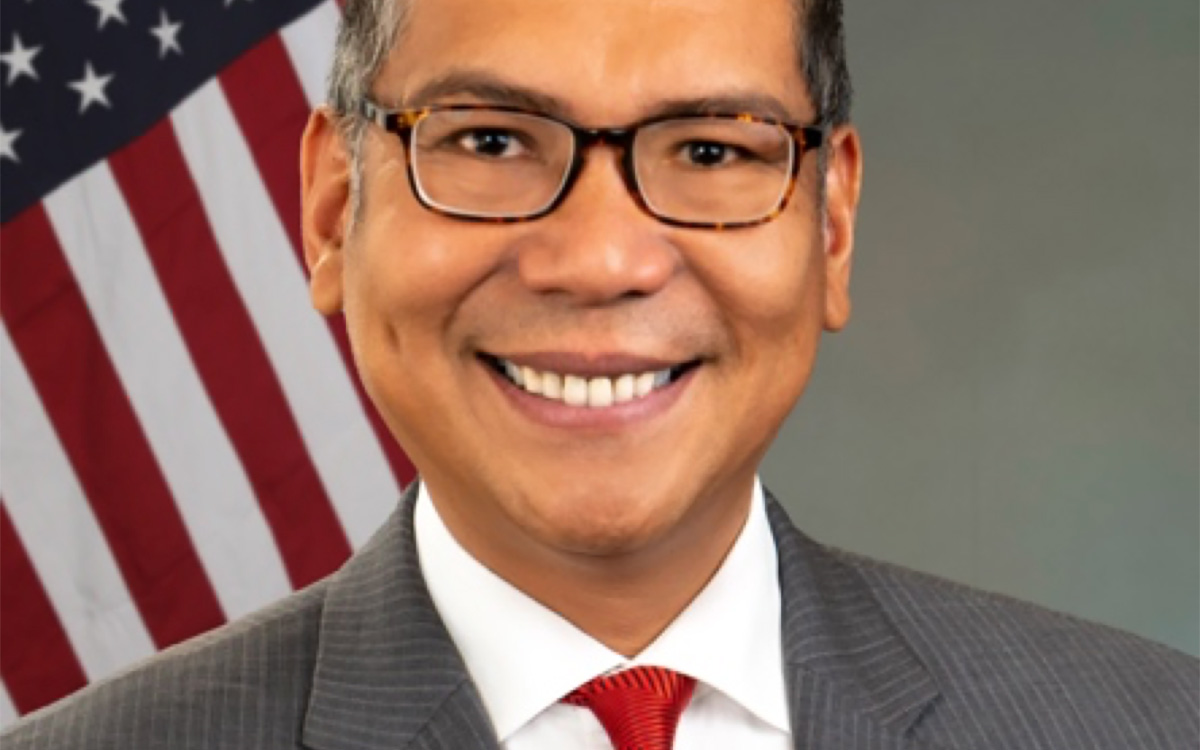
I serve as the only Asian American Pacific Islander member on the U.S. Commission on Civil Rights. And, I am the first and only queer AAPI on the U.S. commission. I am deeply honored to both serve my country and represent my Asian Americans and Pacific Islander community.
Last year, the commission investigated the Federal Response to Anti-Asian Racism in the United States. With congressional authorization, the report documented the experiences of AANHPIs in the U.S. since the dubbing of COVID-19 as the “China Virus” infecting people with the “Kung Flu” by government leadership. Words matter, as this report shows.
This report has a deep personal connection for me. I am the survivor of a hate crime of 25 years ago for being gay, and the victim of a hate crime for being Asian 25 months ago
The Stop AAPI Hate Coalition reported that bias incidents against individuals who are Asian and lesbian, gay, bisexual, transgender or queer (LGBTQ) were most prominent between 2019 and 2022, highlighting the intersectional nature of these incidents. For example, two transgender Asian women stated:
“I was with my new boyfriend at a restaurant. When we walked in the server started calling me names … a b—h, ch—k, tra—i.e. … He said I have a big fat p—s, and told me to go back to China. Then my boyfriend proceeded to walk in the restaurant and when I took a step forward, the server hit me, so I left.”
“Left a restaurant with friends in the Asian district of town. A man began to follow me calling out ‘Hey you f—got c—k!’ and ‘Come here you virus!’ I began to walk fast towards a crowd until he stopped following me.”
To address these and other equally appalling experiences, I helped shepherd the bipartisan Commission on Civil Rights recommendations to the president, Congress, and the nation that:
- Prosecutors and law enforcement should vigorously investigate and prosecute hate crimes and harassment against Asian Americans, as well as Asian Americans who are LGBTQ.
- First responders should be trained to understand what exactly constitutes a hate crime in their jurisdiction, including the protections of LGBTQ people.
- Federal, state, and local law enforcement and victim services should identify deficiencies in their programs for individuals with limited English proficiency.
Greater language access will make an enormous impact for the Asian American community as one in five Asian individuals speak a language other than English at home. A third (34 percent) is limited English proficient. The most frequently spoken languages are Chinese, Korean, Vietnamese, Tagalog, Thai, Khmer, Bengali, Gujarati, Hindi, and Punjabi.
For me, this report comes full circle. Since 1988, I’ve lobbied for passage of LGBTQ-inclusive federal and state laws to prevent hate crimes. Since 2001, I’ve supported South Asian and Muslim victims of post 9/11 violence. In response to the shootings at the Pulse nightclub in Orlando, Fla, in 2016; Atlanta Spa in Georgia in 2021; and Club Q in Colorado Springs, Colo., in 2022, I‘ve trained over 3,000 lawyers, law students, and community leaders on hate crimes law.
And yet, our work is not yet done.
May is Asian Pacific American Heritage Month. June is LGBTQ Pride Month. Despite these challenges, we are resilient. Let us join together in celebrating our Heritage of Pride
Glenn D. Magpantay, Esq., is a long-time civil rights attorney, professor of law and Asian American Studies, and LGBTQ rights activist. Glenn is a founder and former Executive Director of the National Queer Asian Pacific Islander Alliance (NQAPIA). He is principal at Magpantay & Associates: A nonprofit consulting and legal services firm. In 2023, the U.S. Senate (majority) appointed Glenn to the U.S. Commission on Civil Rights to advise Congress and the White House on the enforcement of civil rights laws and development of national civil rights policy.
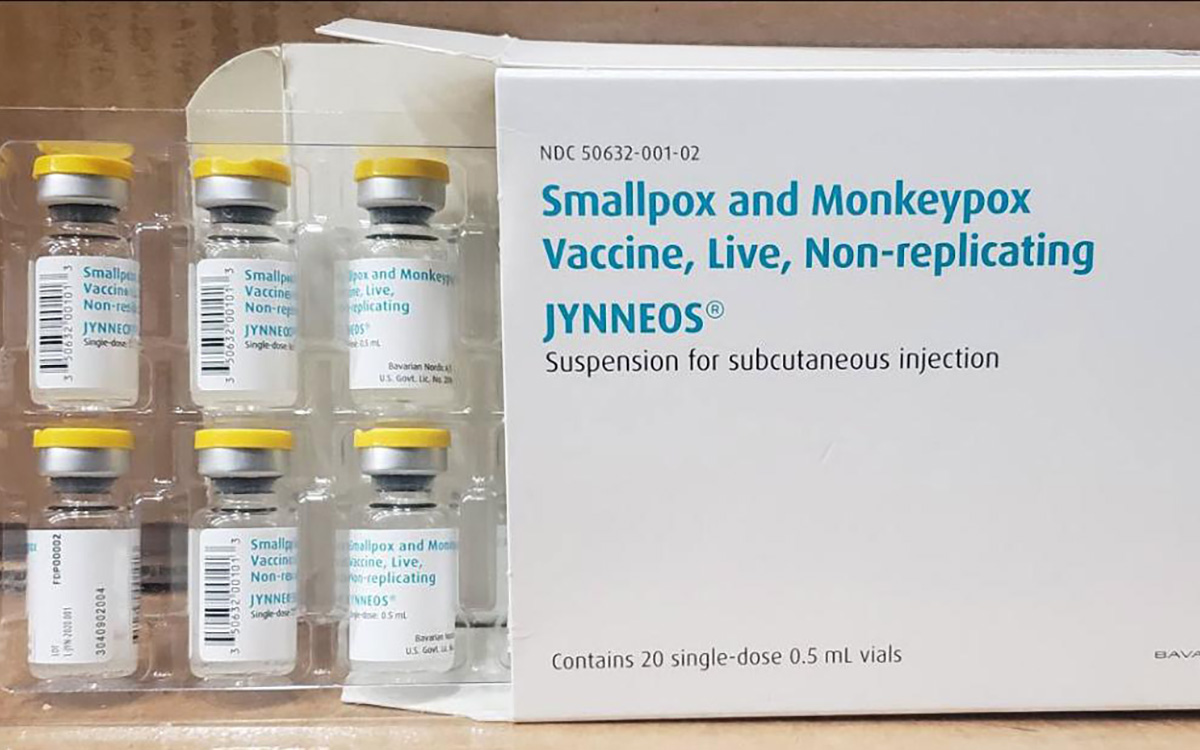
The Centers for Disease Control and Prevention has issued a health advisory regarding a deadlier strain of the Mpox virus outbreak which is currently impacting the Democratic Republic of Congo.
According to the CDC, since January 2023, DRC has reported more than 19,000 suspect mpox cases and more than 900 deaths. The CDC stated that the overall risk to the U.S. posed by the clade I mpox outbreak is low.
The risk to gay, bisexual, and other men who have sex with men who have more than one sexual partner and people who have sex with men, regardless of gender, is assessed as low to moderate the agency stated.
While no cases of that subtype have been identified outside sub-Saharan Africa so far, the World Health Organization said earlier this week that the escalating epidemic in Congo nevertheless poses a global threat, just as infections in Nigeria set off the 2022 outbreak according to a WHO spokesperson.
The spokesperson also noted that as Pride Month and events happen globally, there is more need for greater caution and people to take steps at prevention including being vaccinated.
The CDC advises that while there are no changes to the overall risk assessment, people in the U.S. who have already had mpox or are fully vaccinated should be protected against the type of mpox spreading in DRC. Casual contact, such as might occur during travel, is not likely to cause the disease to spread. The best protection against mpox is two doses of the JYNNEOS vaccine.
The CDC also noted the risk might change as more information becomes available, or if cases appear outside DRC or other African countries where clade I exists naturally.
-

 Canada1 day ago
Canada1 day agoToronto Pride parade cancelled after pro-Palestinian protesters disrupt it
-
 Theater4 days ago
Theater4 days agoStephen Mark Lukas makes sublime turn in ‘Funny Girl’
-

 Baltimore3 days ago
Baltimore3 days agoDespite record crowds, Baltimore Pride’s LGBTQ critics say organizers dropped the ball
-

 Sports4 days ago
Sports4 days agoHaters troll official Olympics Instagram for celebrating gay athlete and boyfriend











